Two weeks ago, the data for cases and hospitalizations in Arizona signaled the state had turned a corner for the progression of coronavirus infections among its residents, but the data for deaths was too incomplete to confirm that milestone had been passed.
Two weeks later, all three major measures of the spread and severity of the SARS-CoV-2 coronavirus confirm the delayed first wave of infections Arizona has experienced has indeed passed through a crest in its coronavirus epidemic, which is now in its rear view mirror. We've continued to refine and update our analysis based on the best estimates of its characteristics, where we've been able to identify significant factors affecting the progression of the coronavirus within the state.
New Hospitalizations Continue Trending Downward
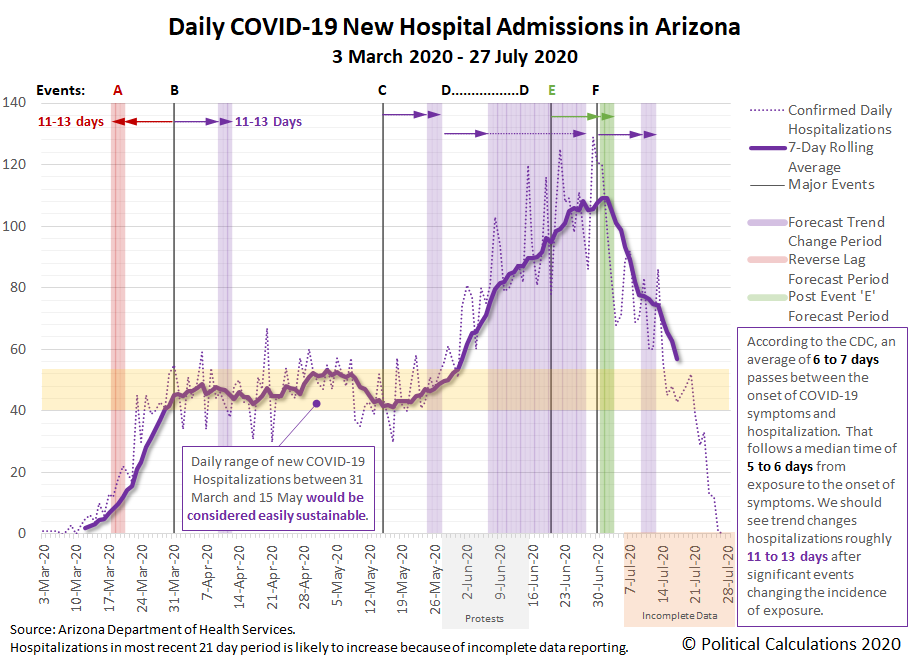
Data for new coronavirus-related hospitalizations in Arizona is especially useful for determining whether particular events affected the rate of exposure to COVID-19 infections within a population.
That's because the date a patient might be admitted to a hospital for health issues associated with a coronavirus infection is independent of any delays in performing COVID tests and the subsequent reporting of their results, which makes it more difficult to use testing-related data for that purpose. The reporting of test results may be affected by shortages of testing supplies and bottlenecks that slow the processing of test results when an unanticipated increase in demand for testing outstrips the capacity of a region's coronavirus testing supply chain to respond.
The CDC reports a median time from exposure to onset of symptoms of 5 to 6 days, with an additional median time of 6 to 7 days before symptoms might become severe enough for an infected person to seek admission to a hospital for treatment. Combined, that gives a stable and narrow median window of 11 to 13 days to use in determining whether a particular event influenced the rate of incidence of exposure to the SARS-CoV-2 coronavirus.
We've used that median window of time in the following chart to indicate when we would expect a change in trend for the rate of new COVID-19 hospitalizations to occur following a significant event (shown as purple or green-shaded vertical bands), or to back calculate when an event would have had to occur to produce an observed change in trend (shown as red-shaded vertical bands).
The downside to using data for new hospitalizations to determine if a given event changed the incidence rate of exposures is that it takes three weeks to get an effectively complete picture of the number of new hospitalizations that occurred on a given date.
We've summarized what we observe in the data in the following table, where the letters correspond to the timing of the significant events indicated on the chart affecting the rate of spread of coronavirus infections in Arizona.
| Timeline of Events Affecting Rate of Spread of COVID-19 Coronavirus in Arizona | |||
|---|---|---|---|
| Event/Date | Description | Observed Change in Trends for Hospitalizations 11-13 Days Later | |
| A 19 Mar 2020 | California imposes statewide lockdown order | Significant change from rising to steady (bounded range) rate of hospitalizations. We think Arizonans effectively implemented practices to minimize their exposure risk to potential coronavirus infections, which then happened to show up as a change in trend immediately after Arizona implemented its own statewide lockdown order. | |
| B 31 Mar 2020 | Arizona imposes statewide lockdown order through April 2020 | Minimal change, new COVID-19 hospitalizations continue within bounded range. We think the main effect of the lockdown order was to standardize how Arizonans minimized their coronavirus exposure risks, which allowed the benefits to extend until the order was lifted, although that came at great economic cost. The lockdown would later be extended to 15 May 2020. | |
| C 15 May 2020 | Arizona lifts statewide lockdown order | Significant change from steady to rising rate of new hospitalizations. | |
| D 28 May 2020 to 15 Jun 2020 | Large scale political protests (Black Lives Matter/George Floyd/Anti-Police) | Change in rate of growth in rate of new hospital admissions as the protests greatly increased the risk and rate of exposure to the coronavirus for younger Arizonans, who are less likely to require hospitalization. Sharp increase in number of cases not requiring hospital admission. | |
| E 19 Jun 2020 | Governor Ducey's executive order allowing counties to require wearing masks in public venues begins to be implemented. | Significant change as new COVID-19 hospital admissions peak and begin to decline. | |
| F30 Jun 2020 | Arizona imposes 'mini-lockdown' order | Minimal change, though data still incomplete for this period. Continued downward trend. | |
One important thing to note for the change in trend associated with the anti-police protests in Arizona's larger cities is that older Arizonans, who are much more likely to require hospitalization and risk death if they become infected by the SARS-CoV-2 coronavirus, appear to have recognized the heightened risk of exposure to the virus from these mass gatherings and have avoided participating in them. Their responsible choices reduced the rate at which hospitalizations for those Age 45 or older were observed to increase during the period where they would be expected to have an effect, while the share of younger Arizonans requiring coronavirus-related hospitalizations increased during this period.
The bigger story however is the peak and reversal in the period associated with Governor Doug Ducey's executive order allowing counties to require residents to wear masks in businesses and other public venues on 18 March 2020 that was quickly implemented in Arizona's four most affected counties on 19 March 2020.
Coming a few days after the anti-police protests petered out, which eliminated a major contributing factor to the spread of coronavirus exposures in Arizona, the governor's mask order appears to have directly contributed to a sharp decline in hospitalizations. It initially appears to be one of the most effective actions taken by any state or local government official during the state's experience with the global coronavirus pandemic.
Before closing this section, we should note that the data for daily new hospital admissions shown in the chart above was obtained on 27 July 2020, prior to a major change in COVID-19 reporting requirements for hospitals in Arizona that revises a large portion of the data. Beginning on 28 July 2020, Arizona's official data began reflecting a new policy where all hospitals in Arizona are now required to report cases to the state, which at this writing, affects data going back to early June 2020. We've presented the pre-revised data because it represents a consistent sample of hospital admissions during the prior reporting periods, without the sudden and incomplete addition of cases counted at those hospitals whose totals are only just now being included in the state's official figures.
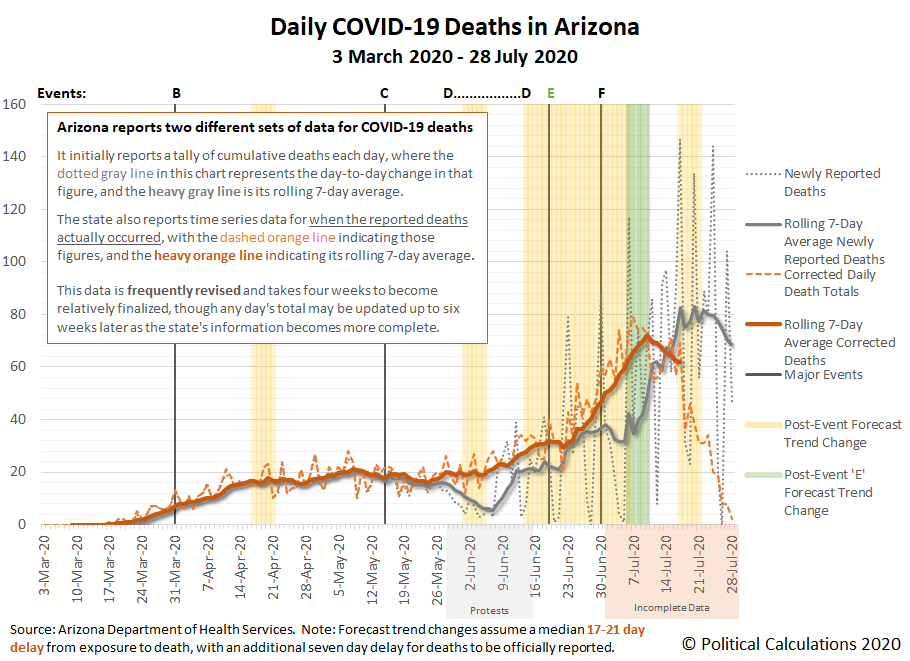
Data for Deaths in Arizona Confirm a Corner Has Been Turned
Data for deaths is similar to that for hospitalizations in that there is a relatively stable window of time that can be used to trace a coronavirus-related death back to the time the ultimately fatal exposure occurred. Unlike the data for hospitalizations, it takes much longer to be realized.
For deaths attributed to COVID-19, the CDC indicates the median time death occurs is 12 to 15 days depending on age following the onset of symptoms, which follows the median period of 5 to 6 days from exposure to symptom onset, which gives a combined median window of 17 to 21 days from initial exposure to death for the affected individuals. On top of that, there is typically a seven day lag in reporting deaths.
In the following chart, we've applied that refined time estimate to project the expected changes in trend for the actual timing of coronavirus-related deaths, finding much of the same pattern we identified from the data for COVID-19 hospitalizations in Arizona.
Here, we confirm upturns in the expected periods following when Arizona lifted its statewide lockdown order and in the period associated with the anti-police protests. This latter surge occurs about 11 days into the forecast period. Since the reported deaths for this period are concentrated the Age 65+ demographic, we think it might be attributable to protest participants exposing older relatives after their initial exposure at the mass gatherings in which they participated.
Although it falls within the period for which officially reported data is still incomplete, there is enough data available to indicate Arizona has turned a corner for deaths during its coronavirus epidemic. The approximate timing falls within the period that would be expected following the end of the anti-police protests and the implementation of Governor Ducey's mask order.
The Spread of New Cases Continues Post-Peak Downward Trend
The data for confirmed cases is the most difficult to use in projecting when a change in trend will occur following a significant event that changes the risk of exposure. While potentially offering the shortest time between exposure and confirmed result, the reporting of results is subject to issues related to the available supply of test kits and bottlenecks in processing. For Arizona, that has meant a growing delay between the time when test specimens are collected after being requested and when a positive result is reported because of the increase in demand for testing related to its surge of coronavirus infections.
Assuming the onset of COVID-19 symptoms following exposure some median 5 to 6 days earlier is what prompts an individual to seek confirmation of a coronavirus infection via testing, the amount of time for an Arizonan to receive results has increased from 9 to 15 days after exposure in May 2020 up to a range of 13 to 19 days in June 2020, and then up to as many as 18 to 24 days after exposure in July 2020. These lags are consistent with what Arizona's Maricopa County has indicated applies for its daily case reporting.
The following chart takes these variable lags into account in projecting when a change in trend might be observed following significant events affecting the risk of exposure.
Once again, the reversal of the upward trend coinciding with the period in which the number of cases are projected to be affected by the timing of Governor Ducey's mask order stands out, with the number of newly confirmed cases falling sharply afterward.
Since this data captures the known extent of active coronavirus cases in Arizona however, it provides a means of approximating the number of additional coronavirus cases that resulted from the anti-police protests in Arizona using its seven-day moving averages. Here, we can use the upward trend in cases that was established following the lifting of Arizona's statewide lockdown order on 15 May 2020 to estimate the number of excess cases related to the protests, those above and beyond the state's initial post-lockdown trendline, which would be anticipated to fall between 11 June 2020 and 2 July 2020.
Doing that math, we find that if the number of new cases had simply risen at the rate indicated by its initial post-lockdown trendline, the state would have added 39,442 cases between these dates. Instead, Arizona added 52,474 cases, with nearly a quarter of this total attributable to the mass gatherings associated with the anti-police protests in this raw estimate.
Comparing the Coronavirus Experiences of Arizona and New York
Since mid-May 2020, Arizona has realized an incidence of cases that is very similar to what New York experienced from February through April 2020. The following chart shows just how similar, and also how different, Arizona's experience has been using the metrics of the daily 7-day average of newly confirmed coronavirus cases per 100,000 residents and the daily 7-day average of deaths attributed to COVID-19 per 100,000 residents.
We confirm both New York and Arizona residents have experienced very similar rates of coronavirus infections. At their peaks, hospitals and health care systems within both states operated at or near 100% of their available capacity before the spreads of their respective coronavirus surges subsided.
Meanwhile, at both states' peak in deaths per 100,000 residents, we confirm New York experienced nearly 3.4 times as many deaths as Arizona. We believe this difference in outcomes is directly attributable to extremely poor policy decisions made in managing the coronavirus epidemic in New York as compared to how Arizona's state and public health officials have managed its similarly sized epidemic surge.
Finally, we should also address the role of politically partisan health care professionals in promoting participation in anti-police protests, who undermined their credibility and responsibilities to protect the public's health by doing so. In failing to "condemn these gatherings as risky for COVID-19 transmission" or to recognize that participants either could not or would not practice the precautions they advised to the general public to guard against virus transmission, their reckless and negligent advocacy sent a loud message that they did not take the precautions they advised seriously. That corrupt message greatly amplified the spread of transmissions in other public venues during the time the protests continued, such as bars, gyms, and public pools and water parks, where many young people in particular felt empowered to similarly disregard the precautions they observed protestors disregarding, both endangering themselves and greatly contributing to the spread of the coronavirus.
Arizona's Coronavirus Crest in the Rear View Mirror
The end of the anti-police protests in Arizona and the state government's mask order combined appear to be responsible for Arizona's turning the corner for the spread of coronavirus infections in its delayed first wave.
Arizona is not the only state experiencing a delayed first wave of coronavirus infections, but its experience and somewhat earlier timing can inform others, such as Florida, which are now passing through their own similarly delayed crests as the U.S. enters a "sustained downward trajectory of virus spread."
Previously on Political Calculations
- The Coronavirus Turns a Corner in Arizona
- A Delayed First Wave Crests in the U.S. and a Second COVID-19 Wave Arrives
- The Coronavirus in Arizona
- A Closer Look at COVID-19 Deaths in Arizona
- The New Epicenter of COVID-19 in the U.S.
- How Long Does a Serious COVID Infection Typically Last?
- How Deadly is the COVID-19 Coronavirus?
- Governor Cuomo and the Coronavirus Models
- How Do False Test Outcomes Affect Estimates of the True Incidence of Coronavirus Infections?
- How Fast Could China's Coronavirus Spread?
References
Arizona Department of Health Services. COVID-19 Data Dashboard. [Online Application/Database].
Maricopa County Coronavirus Disease (COVID-19). COVID-19 Data Archive. Maricopa County Daily Data Reports. [PDF Document Directory, Daily Dashboard].
Stephen A. Lauer, Kyra H. Grantz, Qifang Bi, Forrest K. Jones, Qulu Zheng, Hannah R. Meredith, Andrew S. Azman, Nicholas G. Reich, Justin Lessler. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Annals of Internal Medicine, 5 May 2020. https://doi.org/10.7326/M20-0504.
U.S. Centers for Disease Control and Prevention. COVID-19 Pandemic Planning Scenarios. [PDF Document]. Updated 10 July 2020.
Labels: coronavirus, data visualization, health, risk
Welcome to the blogosphere's toolchest! Here, unlike other blogs dedicated to analyzing current events, we create easy-to-use, simple tools to do the math related to them so you can get in on the action too! If you would like to learn more about these tools, or if you would like to contribute ideas to develop for this blog, please e-mail us at:
ironman at politicalcalculations
Thanks in advance!
Closing values for previous trading day.
This site is primarily powered by:
CSS Validation
RSS Site Feed
JavaScript
The tools on this site are built using JavaScript. If you would like to learn more, one of the best free resources on the web is available at W3Schools.com.